How health care quality varies by state
Free NPI Lookup dug into the 2023 National Healthcare Quality and Disparities report to analyze differences in quality of care between states.
After a period of health care improvements within the United States, the COVID-19 pandemic dramatically slowed its progress. The pandemic worsened patient safety outcomes and exacerbated inequities in the U.S. health system while deprioritizing other major health initiatives, according to a 2024 report by the Centers for Medicare & Medicaid Services.
What's more, over 15 million Medicaid beneficiaries lost coverage following the end of a pandemic-era policy that had automatically re-enrolled recipients. Because state legislatures administer Medicaid, people across the country have felt the impact differently. Still, the situation will likely continue to cause lapses in care overall as patients struggle to renew or find coverage.
In general, the quality of health care varies dramatically throughout the country. To get a broader view of geographic trends, Free NPI Lookup dug into the 2023 National Healthcare Quality and Disparities report to analyze disparities in quality of care between states.
Rankings were based on more than 150 factors, including how easy it is to access services, quality of services, hospital admissions, health conditions, and rates of post-surgery complications. The data was collected between 2016 and 2021.
Though health care spending is much higher in the U.S. than in other countries, the state and federal governments provide lower-quality care than many other industrialized nations. After a long period of increasing longevity, life expectancies in U.S. residents fell to 76 years old in 2021, more than eight years fewer than in Japan.
Unlike many peer nations, the U.S. doesn't provide universal health coverage. As a result, access to insurance (and the risk of losing it) is a crucial factor for Americans' health: Those without health coverage may miss vaccinations, health screenings, and early treatments. Without this preventative care, the uninsured are more prone to develop severe health conditions and have worse outcomes.
Some regional variations exist in health care quality
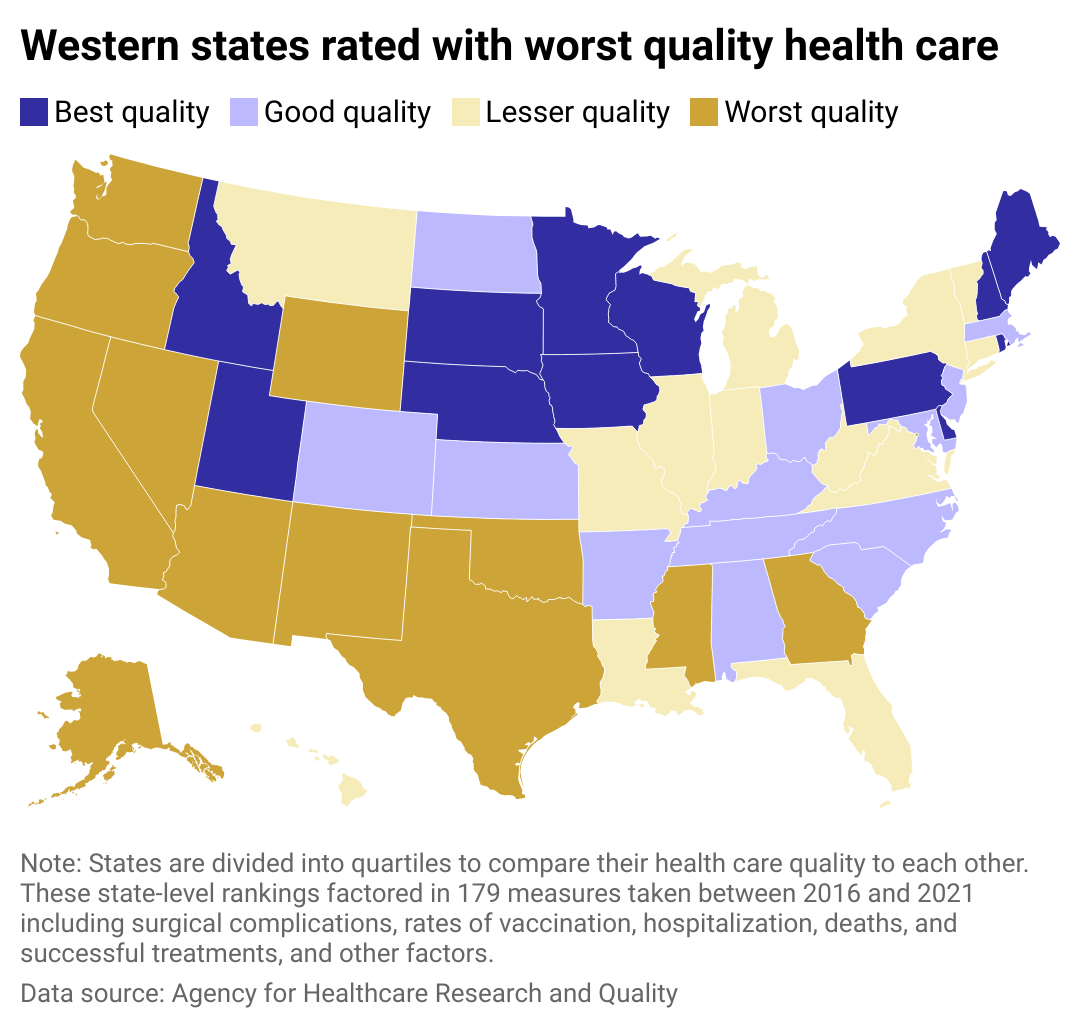
As the availability of clinical services has declined in small towns and rural areas, access to quality care can vary widely between and even within states. It also varies dramatically based on race, socioeconomic factors, and other demographic characteristics.
For instance, low-ranking states like California, Texas, New Mexico, Arizona, and Oklahoma are home to some of the largest Native American and Hispanic and Latino populations, who are among the least likely to have health insurance in the U.S., according to the 2023 National Healthcare Quality and Disparities Report.
Meanwhile, some states that perform well in overall health care quality still have significant disparities in access. Minnesota and Pennsylvania ranked among the highest quality care but had some of the highest disparities across racial and ethnic lines.
These disparities worsen health outcomes within already marginalized communities in the U.S. and shorten their average lifespan by years. The COVID-19 pandemic increased job losses among low-wage service workers, costing some the loss of their employer-sponsored health care and putting essential, public-facing professions such as cashiers and bus drivers at risk.
There is no one-size-fits-all approach to improving quality health care access. While investment in telehealth rose during the pandemic, for instance, those without reliable internet access may be left behind.
For this reason, states have worked with the federal government to increase the number of medical professionals in the field through recruitment and even monetary incentives, reducing shortages in rural and other high-need areas while focusing on culturally competent care.
Story editing by Elsie Drexler. Additional editing by Elena Cox and Kelly Glass. Copy editing by Kristen Wegrzyn.
This story originally appeared on Free NPI Lookup and was produced and distributed in partnership with Stacker Studio.